This pattern is especially damaging for people recovering from abuse because it interacts directly with the brain changes that trauma creates. What feels merely “confusing” to others can be re-traumatising at a neurological level for survivors.
Here’s why — clearly, and without blaming you.
1. Abuse rewires the nervous system toward hyper-vigilance
During abuse, the brain learns:
- closeness can suddenly become unsafe,
- love is unpredictable,
- safety depends on monitoring others’ moods.
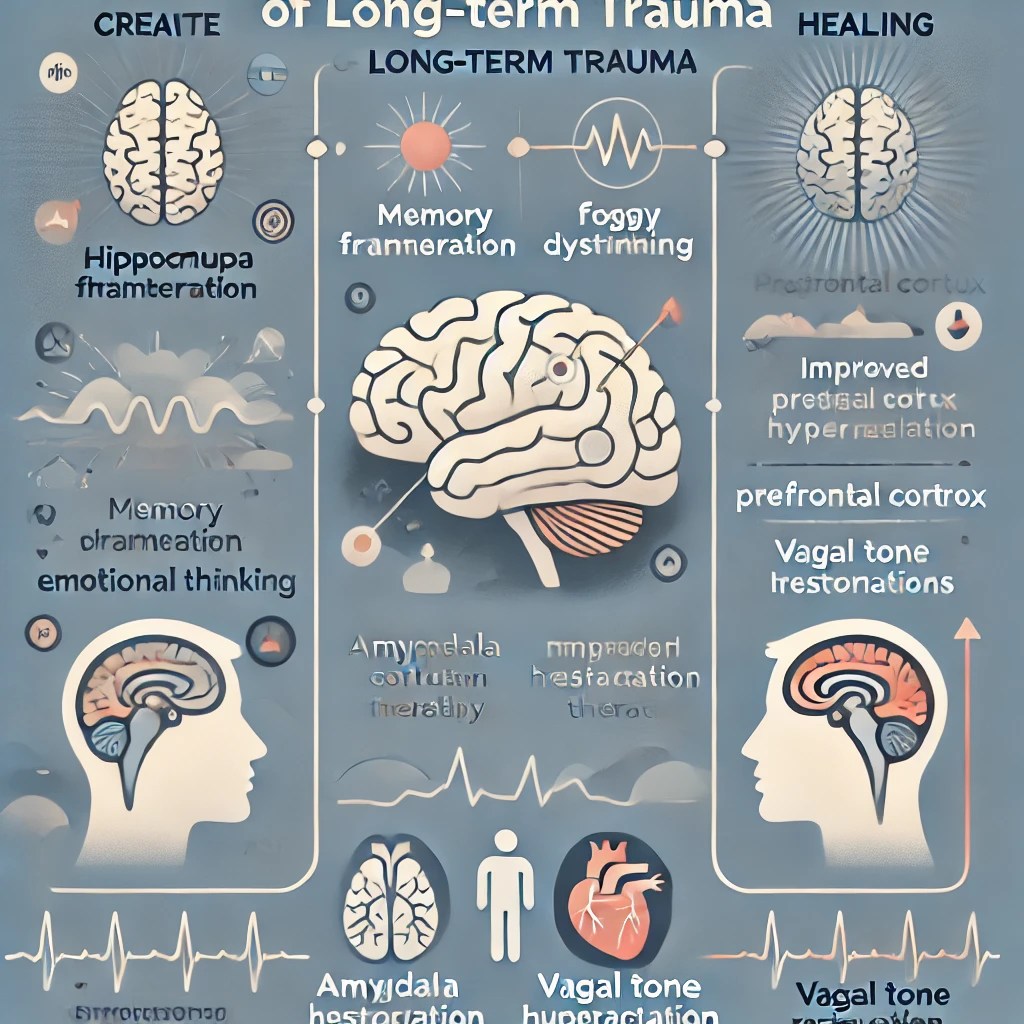
This sensitises the amygdala and weakens trust in internal signals.
So when a partner goes evasive:
- your nervous system doesn’t read it as neutral,
- it reads it as threat recurrence.
Your body reacts before your mind can reassure you.
2. Intermittent withdrawal mimics the abuse cycle
Abusive dynamics often follow:
- Connection
- Tension
- Withdrawal or punishment
- Relief or reunion
Avoidant or deceptive withdrawal — especially around meaningful times — mirrors this exact cycle.
Your brain recognises the pattern even if your conscious mind says:
“This is different.”
That recognition triggers:
- cortisol spikes,
- dopamine crashes,
- intense attachment activation.
This is not emotional weakness. It’s pattern memory.
3. Trauma survivors are trained to self-blame
Abuse conditions the brain to ask:
“What did I do wrong?”
So when someone pulls away:
- you search your behaviour,
- soften your needs,
- wait longer than is healthy,
- rationalise their absence.
Avoidant or deceptive partners unconsciously benefit from this — because you delay boundary-setting.
4. Silence is neurologically louder after abuse
For trauma survivors:
- silence ≠ neutral space
- silence = danger signal
Because in abuse, silence often preceded:
- escalation,
- punishment,
- abandonment,
- gaslighting.
So evasiveness activates the same neural circuitry as past threat.
Your distress is an echo — not an overreaction.
5. Hope keeps the trauma bond alive
Avoidant or deceptive partners often leave:
- just enough warmth,
- just enough ambiguity,
- just enough possibility.
That keeps your dopamine system engaged in “seeking” mode:
Maybe it will go back to how it was.
This is the neurobiology of trauma bonding, even without overt abuse.
6. Healing requires consistency — not intensity
Recovery from abuse depends on:
- predictability,
- repair after rupture,
- emotional follow-through.
Evasive partners offer intensity without reliability, which:
- destabilises regulation,
- slows neural healing,
- keeps your system in survival mode.
You cannot heal in an environment your body still has to scan.
7. The hidden cost: erosion of self-trust
Each time you:
- ignore unease,
- override your instincts,
- wait through silence,
your brain relearns:
“My signals are wrong. I must adapt.”
That is the opposite of trauma recovery.
A grounding truth to hold
Any relationship that requires you to relive the neurological posture of abuse — waiting, wondering, shrinking — is not compatible with healing, regardless of intent.
Safety is not about promises.
It’s about consistency your body can rest in.